Introduction
Geriatric assessment can aid in optimizing treatment strategies and supportive interventions for older adults with diffuse large B-cell lymphoma (DLBCL). Recently, Fondazione Italiana Linforni developed the simplified Geriatric Assessment (sGA) and Elderly Prognostic Index (EPI) to tailor treatment and predict the prognosis of DLBCL in older adults. Herein, we validated the prognostic value of sGA and EPI, and modified the sGA to make it more effective for older DLBCL patients in China.
Methods
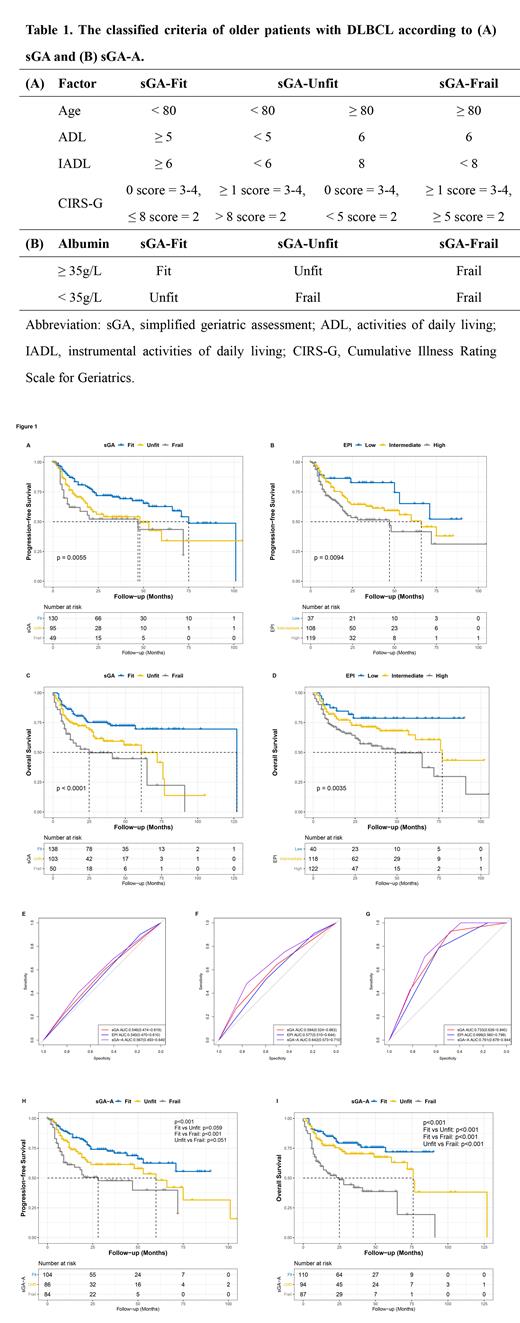
A total of 257 patients with DLBCL aged ≥65 years from Beijing Hospital and Peking University Third Hospital were included in the study. The sGA, which was modified from original geriatric assessment (oGA), incorporates age, activities of daily living (ADL), instrumental ADL, and Cumulative Illness Rating Scale for Geriatrics (CIRS-G), identifying patients into fit, unfit, and frail group. EPI integrated sGA with the IPI score and hemoglobin, identifying patients into low-, intermediate-, and high-risk group. Early mortality was defined as any death occurring within three months from the date of diagnosis. Kaplan-Meier and receiver operating characteristic (ROC) curves were used to assess survival rates and the sensitivity and specificity of the geriatric assessment tools, respectively, whereas the log-rank test was used for comparison. Univariate and multivariate Cox regression analyses were used to identify the independent biomarkers for the patients. Logistics regression analyses were used to analyze the correlation between the geriatric assessment tools and early mortality.
Results
In the study, both sGA and EPI were related to the progression-free survival (PFS; Figure 1A and 1B), overall survival (OS; Figure 1C and 1D), and early mortality of older patients with DLBCL in China (All p < 0.05). Although they had no ability to predict PFS ( p > 0.05; Figure 1E), ROC curves showed that sGA could predict OS ( p = 0.006; AUC: 0.602; 95%CI: 0.530-0.674; Figure 1F), and early mortality ( p = 0.002; AUC: 0.744; 95%CI: 0.634-0.853; Figure 1G) in older patients with DLBCL in China. As for EPI, it also could predict OS ( p = 0.027; AUC: 0.584; 95%CI: 0.512-0.656; Figure 1F) and early mortality ( p = 0.009; AUC: 0.703; 95%CI: 0.590-0.815; Figure 1G).
To make the geriatric tools more effective for older patients with DLBCL in China, albumin, the independent prognostic biomarker for OS of the cohorts, was added into sGA to establish the modified tool sGA-A (Table 1). According to sGA-A, patients were stratified into fit (36.7%), unfit (30.9%), and frail (32.4%) group. However, 1 patient was excluded due to the deficiency of albumin. The sGA-A was associated with age ( p < 0.001), Ann Arbor stage ( p = 0.002), ECOG-PS ( p < 0.001), lactic dehydrogenase (LDH; p = 0.001), IPI score ( p < 0.001), B symptom ( p < 0.001), hemoglobin ( p < 0.001), and albumin ( p < 0.001). Besides, sGA-A was related to PFS ( p < 0.001; Figure 1H), OS (( p < 0.001; Figure 1I), and early mortality ( p = 0.010) of older patients with DLBCL in China. Furthermore, ROC curves showed that sGA-A not only could predict OS ( p < 0.001; ACU: 0.647; 95%CI: 0.577-0.717; Figure 1F), and early mortality (p = < 0.001; AUC: 0.769; 95%CI: 0.679-0.859; Figure 1G), but also could predict PFS ( p = 0.046; AUC:0.577; 95%CI: 0.502-0.652; Figure 1E). In predicting OS, sGA-A was superior to sGA ( p = 0.010), EPI ( p = 0.006). As for early mortality, sGA-A was superior to the EPI ( p = 0.033), but not sGA ( p = 0.520).
Conclusions
In the study, we validated that sGA and EPI could predict OS and early mortality of older patients with DLBCL in China. Based on sGA, we propose sGA-A, which combined sGA and albumin, as an effective tool for geriatric assessment in DLBCL. The sGA-A compensated for the deficits of the sGA and EPI in predicting PFS, and was superior to sGA and EPI in predicting OS and early mortality. However, further investigations on whether sGA-A could guide the treatment may assist clinicians in improve the prognosis of older patients with DLBCL.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal